Overpronation Cause And Treatment
Overpronation is a condition in which the foot rolls excessively down and inward. The arch may elongate and collapse (or ?fall?) and the heel will lean inward. Overpronation should not be confused with pronation. Pronation is a normal motion of the foot during weight bearing and allows the foot to absorb shock as it contacts the ground.

Causes
Congenital "Flat Feet" - an individual may be born with feet that lack an appropriately supportive arch thereby predisposing the individual to this foot condition. Excessive Weight (Obesity) Too much weight on the foot from either obesity or pregnancy may be a factor. Repetitive Impact walking on flat, hard surfaces continuously places unnatural stress on the foot arch.
Symptoms
Common conditions that develop with prolonged overpronation typically include plantar fasciitis, achilles tendonitis, shin splints, posterior tibial stress syndrome and even IT band syndrome. With long term neglect you may see the development of bunyons, foot deformities and early onset of hip and knee arthritis.
Diagnosis
Pronounced wear on the instep side of shoe heels can indicate overpronation, however it's best to get an accurate assessment. Footbalance retailers offer a free foot analysis to check for overpronation and help you learn more about your feet.

Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improperly fitting footwear can lead to additional foot problems.
Surgical Treatment
Subtalar Arthroereisis. Primary benefit is that yje surgery is minimally invasive and fully reversible. the primary risk is a high chance of device displacement, generally not tolerated in adults.
An implant is pushed into the foot to block the excessive motion of the ankle bone. Generally only used in pediatric patients and in combination with other procedures, such as tendon lengthening. Reported removal rates vary from 38% - 100%, depending on manufacturer.
Physiotherapy And Severs Disease
The muscle group at the back of the lower leg is commonly called the calf. The calf comprises of 2 major muscles (known as the gastrocnemius and soleus) both of which insert into the heel bone via the Achilles tendon. In people who have not yet reached skeletal maturity, a growth plate exists where the Achilles tendon inserts into the heel bone. This growth plate is primarily comprised of cartilage. Every time the calf contracts, it pulls on the Achilles tendon which in turn pulls on the heel's growth plate. When this tension is too forceful or repetitive, irritation to the growth plate may occur resulting in pain and sometimes an increased bony prominence at the back of the heel. This condition is called Severs disease. Severs disease is typically seen in children or adolescents during periods of rapid growth. This is because muscles and tendons become tighter as bones become longer. As a result, more tension is placed on the heel's growth plate.
Causes
Sever?s disease is often an overuse injury. It can be caused by playing sports, especially those involving high impact. Sever?s disease can also be linked to growth which can place a stress on the attachment of the Achilles tendon.
Symptoms
Sever's Disease is most commonly seen in physically active girls and boys from ages 10 to 15 years old. These are the years when the growth plate is still ""open,"" and has not fused into mature bone. Also, these are the years when the growth plate is most vulnerable to overuse injuries, which are usually caused by sports activities. The most common symptoms of this disease include. Heel pain in one or both heels. Usually seen in physically active children, especially at the beginning of a new sports season. The pain is usually experienced at the back of the heel, and includes the following areas. The back of the heel (that area which rubs against the back of the shoe). The sides of the heel. Actually, this is one of the diagnostic tests for Sever's Disease, squeezing the rear portion of the heel from both sides at the same time will produce pain. It is known as the Squeeze Test.
Diagnosis
In Sever's disease, heel pain can be in one or both heels. It usually starts after a child begins a new sports season or a new sport. Your child may walk with a limp. The pain may increase when he or she runs or jumps. He or she may have a tendency to tiptoe. Your child's heel may hurt if you squeeze both sides toward the very back. This is called the squeeze test. Your doctor may also find that your child's heel tendons have become tight.
Non Surgical Treatment
The immediate goal of treatment is pain relief. Because symptoms generally worsen with activity, the main treatment for Sever's disease is rest, which helps to relieve pressure on the heel bone, decreasing swelling and reducing pain. As directed by the doctor, a child should cut down on or avoid all activities that cause pain until all symptoms are gone, especially running barefoot or on hard surfaces because hard impact on the feet can worsen pain and inflammation. The child might be able to do things that do not put pressure on the heel, such as swimming and biking, but check with a doctor first.
What Are The Major Causes Of Posterior Tibial Tendon Dysfunction ?
Overview
There are some things that gain value as they age. Antique dealers are always on the lookout for pieces that have a certain ?wear and tear? look that will bring a high price tag. Our feet on the other hand, don?t always fair as well when they have experienced a lot of wear and tear. Cumulative stress and impact can cause your foot structure to weaken and become prone to injury, especially when you have a flat foot. This is the case with a condition called posterior tibial tendon dysfunction. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot. Sometimes this can be a result of specific trauma, but usually the tendon becomes injured from wear and tear over time. This is more prevalent in individuals with an inherited flat foot but excessive weight, age, and level of activity are also contributing factors.
Symptoms
Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area. Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot. Asymmetrical collapsing of the medial arch on the affected side.
Diagnosis
First, both feet should be examined with the patient standing and the entire lower extremity visible. The foot should be inspected from above as well as from behind the patient, as valgus angulation of the hindfoot is best appreciated when the foot is viewed from behind. Johnson described the so-called more-toes sign: with more advanced deformity and abduction of the forefoot, more of the lateral toes become visible when the foot is viewed from behind. The single-limb heel-rise test is an excellent determinant of the function of the posterior tibial tendon. The patient is asked to attempt to rise onto the ball of one foot while the other foot is suspended off the floor. Under normal circumstances, the posterior tibial muscle, which inverts and stabilizes the hindfoot, is activated as the patient begins to rise onto the forefoot. The gastrocnemius-soleus muscle group then elevates the calcaneus, and the heel-rise is accomplished. With dysfunction of the posterior tibial tendon, however, inversion of the heel is weak, and either the heel remains in valgus or the patient is unable to rise onto the forefoot. If the patient can do a single-limb heel-rise, the limb may be stressed further by asking the patient to perform this maneuver repetitively.
Non surgical Treatment
Depending on the stage of the deformity and patient?s functional goals, various treatment options are available. Some patients improve with conservative care which includes rest and immobilization, shoe modifications, orthoses and bracing, or physical therapy. Surgery might be warranted for advanced stages of the condition. Often a combination of procedures including tendon and muscle augmentation, tendon transfers, realigning of bones or fusion of certain joints might be necessary in more advanced cases. Your doctor will evaluate and recommend an individualized plan of care with your specific needs in mind. 
Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.
Heel Soreness The Causes, Warning Signs And Therapy Methods

The most common form of Heel Pain, is pain on the bottom of the heel. It tends to occur for no apparent reason and is often worse when first placing weight on the foot. Patients often complain of pain the first thing in the morning or after getting up to stand after sitting. The pain can be a sharp, searing pain or present as a tearing feeling in the bottom of the heel. As the condition progresses there may be a throbbing pain after getting off your feet or there may be soreness that radiates up the back of the leg. Pain may also radiate into the arch of the foot.
Causes
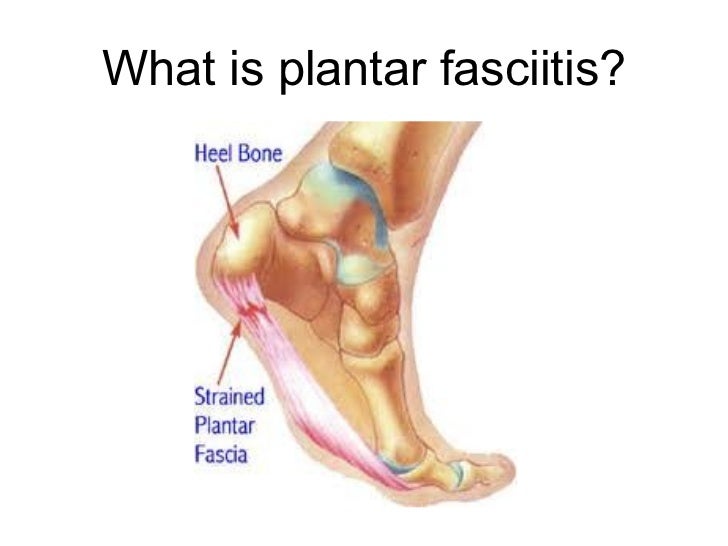
Heel pain can have many causes but the vast majority is caused by plantar fasciitis. Plantar means, ?bottom of the foot.? Fascia is a ligament or ?bundle? of ligaments. The plantar fascia is the thick ligament that helps to hold up the foot and provide spring in our step. Plantar fasciitis is an inflammation of the plantar fascia and causes more than 90% of heel pain among adults in the US. Plantar fasciitis can be acute, that is, as simple strain of the ligament but often is chronic, hanging on for months if not years. Why does that happen? The answer is poor foot mechanics, the foot sinking down too far allowing the plantar fascia to overstretch with each step taken.
Symptoms
The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process the surgeon rules out all the possible causes for your heel pain other than plantar fasciitis. In addition, diagnostic imaging studies such as x-rays or other imaging modalities may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Non Surgical Treatment
If the plantar fasciitis is acute, that is, a sprain of the plantar fascia then it is basically treated as a sprain, with anti-inflammatory drugs, ice, rest, possibly physical therapy. If chronic, the poor foot mechanics need be addressed. Foot mechanics are changed by use of specially moulded shoe inserts known as orthotics. Someone with plantar fasciitis needs an orthotic designed to relieve strain on the plantar fascia. Orthotics are often confused with arch supports. Arch supports, by holding up the arch can remove some of the tension from the plantar fascia. Orthotics, on the other hand, do most of their work on the heel and ball of the foot repositioning the foot for maximized function. What can you do before you see the foot doctor? First, try doing your own version of deep tissue massage by rolling a frozen cola bottle or can from the heel forward into the arch. Do it gently. Do stretching but the key to good stretching is not to stretch too hard so generally avoid weight bearing (standing) stretches but sit on a soft surface like your bed and pull the foot backward on the leg as far as it will go, holding for 20 seconds and relaxing for 5 seconds. Each 25 second ?set? can be repeated 5 times and you have invested about 2 minutes in giving yourself a lot of help. Watch out for the shoes you wear. It is tempting to obtain shoes that are colorful and soft. Here is the proof that soft shoes are bad. Wrap a pillow around your foot with duct tape and walk for a block or two. You will come back with your foot hurting more because your foot sank down deeper into the soft surface, allowing the ligament to stretch more. The shoes should be stiff in the shank and flexible at the ball. Such shoes, to running buffs, are known as motion control shoes or stability shoes so going to one of the small specialty running shoes stores is a good place to start. If you don?t have a desk job, or have an industrial job see if light duty is available. A note from your doc may be all that is required in most cases and most doctors are happy to oblige.
Surgical Treatment
When a diagnosis of plantar fasciitis is made early, most patients respond to conservative treatment and don?t require surgical intervention. Often, when there is a secondary diagnosis contributing to your pain, such as an entrapped nerve, and you are non-responsive to conservative care, surgery may be considered. Dr. Talarico will discuss all options and which approach would be the most beneficial for your condition.
Prevention

Wearing real good, supportive shoes are a great way to avoid heel pain. Usually, New Balance is a good shoe to wear, just for everyday shoe gear. By wearing proper footwear and performing thorough stretches, athletes can help prevent frequent heel pain. If you are starting to get a little discomfort or pain in the feet or heel, know that pain is not normal. So if you are having pain, you should be proactive and visit our office. If you let heel pain get out of control you could run into several other problems. It is always suggested to visit a podiatrist whenever you are experiencing pain.
Concerning Achilles Tendonitis
 Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Causes
Achilles tendinitis is usually caused by straining the Achilles tendon through intense activity or a sudden increase in exercise. Individuals who play basketball often develop Achilles tendinitis as a result of pivoting, jumping, and running. These repetitive movements put pressure on the tendon and can gradually wear it down over time. Increasing the intensity of your workouts may also lead to the development of Achilles tendinitis. This is commonly seen in long distance runners who do quite a bit of uphill running. Similarly, if you start exercising more frequently you may also develop the condition due to overuse of the tendon. Not stretching properly before exercise can also make the tendon more prone to injury. Achilles tendinitis is also common in individuals whose feet have a flattened arch, as this places more stress on the tendon. The condition can also be triggered by arthritis, as joint pain can cause one to compensate by putting more pressure on the Achilles tendon.
Symptoms
Signs and symptoms of Achilles Tendinitis generally include pain and stiffness along your achilles tendon, especially in the morning. Pain in the back of your heel that gets worse with activity. Severe pain the day after exercising. Swelling that gets worse with activity. If you feel a pop in the back of your heel or bottom of you calf, you may have ruptured or torn you achilles tendon.
Diagnosis
On examination, an inflamed or partially torn Achilles tendon is tender when squeezed between the fingers. Complete tears are differentiated by sudden, severe pain and inability to walk on the extremity. A palpable defect along the course of the tendon. A positive Thompson test (while the patient lies prone on the examination table, the examiner squeezes the calf muscle; this maneuver by the examiner does not cause the normally expected plantar flexion of the foot).
Nonsurgical Treatment
Take a course (5 - 7 days) of non-steroidal anti-inflammatory drugs(ibuprofen/voltaren/cataflam/mobic) available from your general practitioner or pharmacist. Apply ice to the Achilles - for 10 minutes every 2 hours, in order to reduce the inflammation. Avoid weight-bearing activities and keep foot elevated where possible. Self-massage - using arnica oil or anti-inflammatory gel. Rub in semi-circles in all directions away from the knotted tissue, three times a day once the nodule is gone, stretch the calf muscle gently do not start running until you can do heel raises and jumping exercises without pain return to running gradually full recovery is usually between six to eight weeks.

Surgical Treatment
Surgery is considered when non-operative measures fail. Patient compliance and postoperative management is an important aspect of the operative management to prevent ankle stiffness or recurrence of the symptoms. Surgery usually requires a removal of the damaged tissue (debridement) and meticulous repair of the tendon. Post-operative immobilization is required, followed by gradual range of motion and strengthening exercises start. It may require 6 months for the full recovery. Some known complication are recurrence, stiffness of the ankle and deep vein thrombosis.
Prevention
The following measures can significantly reduce the risk of developing Achilles tendonitis. Adequately stretch and warm up prior to exercise. Warm down and stretch after exercise. Choose footwear carefully and use footwear appropriate to the sport being undertaken. Use orthotic devices in footwear to correctly support the foot. Exercise within fitness levels and follow a sensible exercise programme. Develop strong, flexible calf muscles.
What Is Heel Discomfort And Ways To Treat It
Overview
The plantar fascia is a band of connective tissue on the bottom of the foot that helps form the arch of the foot. Acute injury or cumulative trauma to the plantar fascia can be a cause of inflammation and heel pain. This is called plantar fasciitis.
Causes
It is common to see patients with Plantar Fasciitis who have been wearing shoes that are too soft and flexible. The lack of support can be stressful on the heel for those patients who’s feet aren’t particularly stable. If these ill fitting shoes are worn for long enough, the stress will lead to Heel Pain as the inflammation of the fascia persists. Footwear assessment and advice will be essential in order to get on top of the Plantar Fasciitis. It may surprise some people to learn that high heeled shoes are not the cause of Plantar Fasciitis, although they can cause tight calf muscles. High arches can lead to Plantar Fasciitis. This is due to the lack of contact under the sole of the foot. Even sports shoes which appear to have good arch support inside are often too soft and not high enough to make contact with the arch of the foot. Hence, the plantar fascia is unsupported. This can lead to Heel pain and Plantar Fasciitis. Flat feet can lead to Plantar Fasciitis. Flat feet is caused by ligament laxity and leads to foot instability. Other structures such as muscles, tendons and fascia work harder to compensate for this instability. Heel pain or Plantar Fasciitis arises when the instability is too great for these other structures to cope with. The strain on the fascia is too severe and the inflammation sets in. Over stretching can lead to Plantar Fasciitis. Certain calf stretches put the foot into a position that creates a pulling sensation through the sole of the foot. This can cause Plantar Fasciitis which can cause pain in the arch of the foot as well as Heel Pain.
Symptoms
Plantar fasciitis is the inflammation of the plantar fascia - a band of tough fibrous tissue running along the sole of the foot. It occurs when small tears develop in the plantar fascia, leading to inflammation and heel pain. The plantar fascia tissue branches out from the heel like a fan, connecting the heel bone to the base of the toes. When the foot moves, the plantar fascia stretches and contracts. The plantar fascia helps to maintain the arch of the foot in much the same way that the string of a bow maintains the bow's arch. The most notable symptom of plantar fasciitis is heel pain. This is typically most severe in the middle of the heel though it may radiate along the sole of the foot. The pain is most often felt when walking first thing in the morning or after a period of rest. As walking continues the pain may decrease; however some degree of pain remains present on movement. The pain may disappear when resting, as the plantar fascia is relaxed. Redness, swelling and warmth over the affected area may also be noticed. The onset of plantar fasciitis is gradual and only mild pain may be experienced initially. However, as the condition progresses the pain experienced tends to become more severe. Chronic plantar fasciitis may cause a person to change their walking or running action, leading to symptoms of discomfort in the knee, hip and back.
Diagnosis
Your doctor may look at your feet and watch the way you stand, walk and exercise. He can also ask you questions about your health history, including illnesses and injuries that you had in your past. The symptoms you have such as the pain location or when does your foot hurts most. Your activity routine such as your job, exercise habits and physical activities preformed. Your doctor may decide to use an X-ray of your foot to detect bones problems. MRI or ultrasound can also be used as further investigation of the foot condition.
Non Surgical Treatment
Biomechanical plantar fasciitis can be easily reduced by correcting misalignment of the feet. Wearing orthopedic shoes for plantar fasciitis and orthotic inserts is an easy, effective method of naturally realigning the foot. Worn consistently from first thing in the morning to last thing at night, orthotic support can reduce and sometimes eliminate plantar fasciitis. Biomechanical plantar fasciitis can be easily reduced by correcting misalignment of the feet. Wearing orthopedic shoes for plantar fasciitis and orthotic inserts is an easy, effective method of naturally realigning the foot. Worn consistently from first thing in the morning to last thing at night, orthotic support can reduce and sometimes eliminate plantar fasciitis. Preserve Your Arch with Strengthening Exercises. While seated and barefoot, squeeze your foot as if you have a small marble under the ball of your foot. If you just happen to have a few marbles handy, you can actually practice picking them up between your toes and ball of your foot - and then set them down again. This stretches and helps strengthen the muscles that run under metatarsals (the longest bones in the foot which create its arched shape). Slowly Increase Physical Activity. If you're a runner, a tried and true method of preventing over-use injuries is to only increase your mileage by 10% weekly, max. If you’re new to a walking program, the same caution should be exercised. Ice and Rest. After mild stretching, use a frozen water bottle to roll under the arch of your foot for 10-20 minutes. It may be possible to make an active recovery by wearing Orthaheel Technology to keep your feet naturally aligned, therefore reducing strain on the plantar fascia, while moving throughout your day.

Surgical Treatment
The most dramatic therapy, used only in cases where pain is very severe, is surgery. The plantar fascia can be partially detached from the heel bone, but the arch of the foot is weakened and full function may be lost. Another surgery involves lengthening the calf muscle, a process called gastrocnemius recession. If you ignore the condition, you can develop chronic heel pain. This can change the way you walk and cause injury to your legs, knees, hips and back. Steroid injections and some other treatments can weaken the plantar fascia ligament and cause potential rupture of the ligament. Surgery carries the risks of bleeding, infection, and reactions to anesthesia. Plantar fascia detachment can also cause changes in your foot and nerve damage. Gastrocnemius resection can also cause nerve damage.
Prevention
It is not always possible to prevent heel pain, but there are measures you can take to help avoid further episodes. Healthy weight. Being overweight can place excess pressure and strain on your feet, particularly on your heels. This increases the risk of damaging your feet and heels. If you are overweight, losing weight and maintaining a healthy weight by combining regular exercise with a healthy, balanced diet can be beneficial for your feet. You can calculate your body mass index (BMI) to find out whether you are a healthy weight for your height and build. To work out your BMI, divide your weight in kilograms by your height in metres squared. A BMI of less than 18.5 means that you are underweight, 18.5-24.9 means that your weight is healthy, 25-29 means that you are overweight, 30-40 means that you are obese, over 40 means that you are morbidly obese. You can also use the BMI healthy weight calculator to work out your BMI. Healthy feet. You should always wear footwear that is appropriate for your environment and day-to-day activities. Wearing high heels when you go out in the evening is unlikely to be harmful. However, wearing them all week at work may damage your feet, particularly if your job involves a lot of walking or standing. Ideally, you should wear shoes with laces and a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels.
What Is Heel Discomfort And Tips To Successfully Treat It

Overview
Plantar fasciitis is one of the most common sources of heel pain. Your plantar fascia is a thick fibrous band of connective tissue originating on the bottom surface of the calcaneus (heel bone) and extending along the sole of the foot towards the toes. Your plantar fascia acts as a passive limitation to the over flattening of you arch. When your plantar fascia develops micro tears or becomes inflammed it is known as plantar fasciitis.
Causes
Factors which may contribute to plantar fasciitis and heel spurs include a sudden increase in daily activities, increase in weight (not usually a problem with runners), or a change of shoes. Dramatic increase in training intensity or duration may cause plantar fasciitis. Shoes that are too flexible in the middle of the arch or shoes that bend before the toe joints will cause an increase in tension in the plantar fascia. Even though you may have run in shoes that are flexible before, now that you have developed plantar fasciitis, make certain that your shoe is stable and does not bend in the midfoot. Check and be certain that your shoes are not excessively worn. Shoes that do not sufficiently control excessive pronation combined with an increase in training can lead to this condition. A change in running style or parameters, such as starting speed work, running on the ball of your foot or sudden increase in hill workouts may lead to problems. All changes should be gradual and not abrupt. Gait changes such as altering your foot strike, switching shoe style, running barefoot or in minimalist shoes should all be made gradually and not abruptly. The "terrible too's" of too much, too soon, too often with too little rest also applies to "too many changes with too little adaptation". Make your changes gradually and allow your muscles, bones, and other body structures to adapt to the alterations you may be attempting.
Symptoms
The heel pain characteristic of plantar fasciitis is usually felt on the bottom of the heel and is most intense with the first steps of the day. Individuals with plantar fasciitis often have difficulty with dorsiflexion of the foot, an action in which the foot is brought toward the shin. This difficulty is usually due to tightness of the calf muscle or Achilles tendon, the latter of which is connected to the back of the plantar fascia. Most cases of plantar fasciitis resolve on their own with time and respond well to conservative methods of treatment.
Diagnosis
Plantar fasciitis is usually diagnosed by a health care provider after consideration of a person’s presenting history, risk factors, and clinical examination. Tenderness to palpation along the inner aspect of the heel bone on the sole of the foot may be elicited during the physical examination. The foot may have limited dorsiflexion due to tightness of the calf muscles or the Achilles tendon. Dorsiflexion of the foot may elicit the pain due to stretching of the plantar fascia with this motion. Diagnostic imaging studies are not usually needed to diagnose plantar fasciitis. However, in certain cases a physician may decide imaging studies (such as X-rays, diagnostic ultrasound or MRI) are warranted to rule out other serious causes of foot pain. Bilateral heel pain or heel pain in the context of a systemic illness may indicate a need for a more in-depth diagnostic investigation. Lateral view x-rays of the ankle are the recommended first-line imaging modality to assess for other causes of heel pain such as stress fractures or bone spur development. Plantar fascia aponeurosis thickening at the heel greater than 5 millimeters as demonstrated by ultrasound is consistent with a diagnosis of plantar fasciitis. An incidental finding associated with this condition is a heel spur, a small bony calcification on the calcaneus (heel bone), which can be found in up to 50% of those with plantar fasciitis. In such cases, it is the underlying plantar fasciitis that produces the heel pain, and not the spur itself. The condition is responsible for the creation of the spur though the clinical significance of heel spurs in plantar fasciitis remains unclear.
Non Surgical Treatment
More than 90% of patients with plantar fasciitis will improve within 10 months of starting simple treatment methods. Rest. Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running or step aerobics). Ice. Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day. Nonsteroidal anti-inflammatory medication. Drugs such as ibuprofen or naproxen reduce pain and inflammation. Using the medication for more than 1 month should be reviewed with your primary care doctor. Exercise. Plantar fasciitis is aggravated by tight muscles in your feet and calves. Stretching your calves and plantar fascia is the most effective way to relieve the pain that comes with this condition. Cortisone injections. Cortisone, a type of steroid, is a powerful anti-inflammatory medication. It can be injected into the plantar fascia to reduce inflammation and pain. Your doctor may limit your injections. Multiple steroid injections can cause the plantar fascia to rupture (tear), which can lead to a flat foot and chronic pain. Soft heel pads can provide extra support. Supportive shoes and orthotics. Shoes with thick soles and extra cushioning can reduce pain with standing and walking. As you step and your heel strikes the ground, a significant amount of tension is placed on the fascia, which causes microtrauma (tiny tears in the tissue). A cushioned shoe or insert reduces this tension and the microtrauma that occurs with every step. Soft silicone heel pads are inexpensive and work by elevating and cushioning your heel. Pre-made or custom orthotics (shoe inserts) are also helpful. Night splints. Most people sleep with their feet pointed down. This relaxes the plantar fascia and is one of the reasons for morning heel pain. A night splint stretches the plantar fascia while you sleep. Although it can be difficult to sleep with, a night splint is very effective and does not have to be used once the pain is gone. Physical therapy. Your doctor may suggest that you work with a physical therapist on an exercise program that focuses on stretching your calf muscles and plantar fascia. In addition to exercises like the ones mentioned above, a physical therapy program may involve specialized ice treatments, massage, and medication to decrease inflammation around the plantar fascia. Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged plantar fascia tissue. ESWT has not shown consistent results and, therefore, is not commonly performed. ESWT is noninvasive-it does not require a surgical incision. Because of the minimal risk involved, ESWT is sometimes tried before surgery is considered.

Surgical Treatment
In very rare cases plantar fascia surgery is suggested, as a last resort. In this case the surgeon makes an incision into the ligament, partially cutting the plantar fascia to release it. If a heel spur is present, the surgeon will remove it. Plantar Fasciitis surgery should always be considered the last resort when all the conventional treatment methods have failed to succeed. Endoscopic plantar fasciotomy (EPF) is a form of surgery whereby two incisions are made around the heel and the ligament is being detached from the heel bone allowing the new ligament to develop in the same place. In some cases the surgeon may decide to remove the heel spur itself, if present. Just like any type of surgery, Plantar Fascia surgery comes with certain risks and side effects. For example, the arch of the foot may drop and become weak. Wearing an arch support after surgery is therefore recommended. Heel spur surgeries may also do some damage to veins and arteries of your foot that allow blood supply in the area. This will increase the time of recovery.
Prevention
Make sure you wear appropriate supportive shoes. Don't over-train in sports. Make sure you warm up, cool down and undertake an exercise regime that helps maintain flexibility. Manage your weight, obesity is a factor in causing plantar fasciitis. Avoid walking and running on hard surfaces if you are prone to pain. You should follow the recognized management protocol - RICED-rest, ice, compression, elevation and diagnosis. Rest, keep off the injured ankle as much as possible. Ice, applied for 20 minutes at a time every hour as long as swelling persists. Compression, support the ankle and foot with a firmly (not tightly) wrapped elastic bandage. Elevation, keep foot above heart level to minimize bruising and swelling. Diagnosis, Consult a medical professional (such as a Podiatrist or doctor) especially if you are worried about the injury, or if the pain or swelling gets worse. If the pain or swelling has not gone down significantly within 48 hours, also seek treatment. An accurate diagnosis is essential for proper rehabilitation of moderate to severe injuries.